Outsmarting Chronic Pain: Proven Strategies for Lasting Relief
Understanding Chronic Pain: More Than Just a Physical Sensation
Anyone living with chronic pain knows it transcends physical sensation to become a complex neurological experience that fundamentally alters how you experience the world. My reckoning began unexpectedly at age 28, with a seemingly innocuous bout of dry eyes that gradually transformed into a relentless battle with neuropathic corneal pain, a rare condition where damaged corneal nerves become hypersensitive to every fluctuation in temperature, humidity and lighting.
Over six years, I navigated a labyrinth of treatments with little to show for it. I had my tear ducts plugged, then cauterized to retain moisture on the parched surface of my eyes. When this failed to provide adequate relief, I consulted third and fourth dry eye specialists, spending hundreds on pharmaceutical drops, procedures, and medications that failed to do anything but deplete my bank account. As my condition worsened, I was forced to don goggles day and night to reduce my exposure to moving air.
After exhausting mainstream medicine's offerings, I widened my search, visiting naturopaths and acupuncturists and spending thousands more on supplements and intensive detox protocols. I exchanged my pharmaceutical drops for herbal rinses and salves. I tried meditation, intensive elimination diets, breathing exercises and cold immersion. None of it was the silver bullet I desperately sought. My unraveling became a hidden spectacle of desperate endurance and daily pain management.
The Neuroplastic Revolution: Rethinking Pain Management
A major turning point in my healing journey came through an unexpected source: understanding neuroplasticity. Dr. Norman Doidge's groundbreaking 2015 book, The Brain's Way of Healing, introduced me to a revolutionary concept: our brains are not static organs, but dynamic systems capable of reorganizing themselves in response to persistent experiences.
Neurons "rewire" themselves by altering connections at the synapse, either strengthening or weakening the links between them. As a result of my prolonged pain, my brain had become highly efficient at processing it, becoming hypersensitive and recruiting neighboring nerve endings to assist in the task.
The Mind-Body Connection in Chronic Pain
Neuroplasticity operates on a fundamental principle: neurons that fire together, wire together. In chronic pain conditions, this means that repeated pain signals can train the brain to become increasingly efficient at processing pain. Remarkably, up to 25% of neurons in certain brain regions can become dedicated to pain processing, creating a self-perpetuating cycle of discomfort.
Many of the areas in our brain involved in pain processing are also responsible for processing thoughts, sensations, images, memories, movements, emotions, and beliefs. This insight helps explain why pain can impair our ability to concentrate and think clearly, sensitizing us to certain sounds and lights, hindering our physical coordination causing us to be irritable and have emotional outbursts.
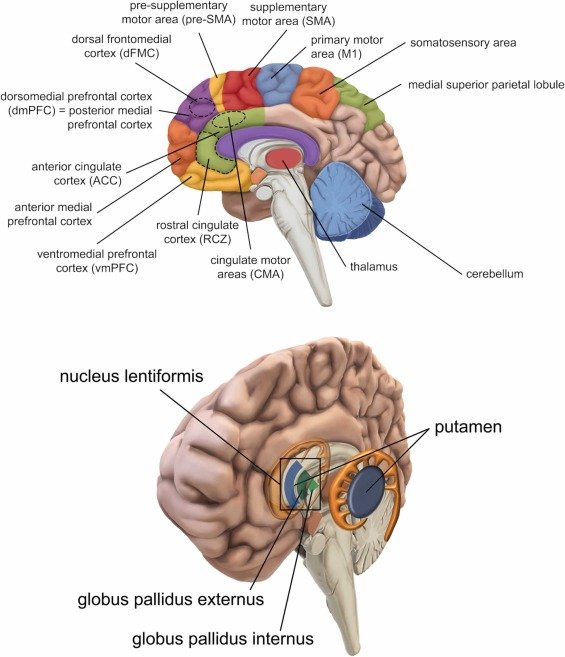
These are two key brain regions involved in pain:
S1 (Primary Somatosensory Cortex): Represents the location and intensity of pain signals in the body. S1 sits in the parietal lobe, specifically along the postcentral gyrus—a ridge right behind the central sulcus, which is the deep groove separating the frontal and parietal lobes.
ACC (Anterior Cingulate Cortex): Handles the emotional and motivational component of pain. The ACC lies deeper, positioned near the brain's midline, forward of the parietal areas, and wraps around like a collar handling emotional processing.
Evidence-Based Strategies for Neural Rehabilitation
Inspired by Dr. Michael Moskowitz’s research, I undertook a multifaceted strategy for neural rehabilitation consisting of two primary principles:
1. Sensory Redirection Techniques
The brain processes pain through multiple sensory pathways. By intentionally introducing alternative sensory experiences through light, sound, scent, temperature, vibration, and movement we can effectively "compete" with pain signals, gradually reducing neural hypersensitivity.
A 2025 pilot study in the Journal of Medical Internet Research tested whether multisensory therapy could help nursing home residents manage pain. Participants received four 20-minute sessions each week in a special "Snoezelen room"—a calming space with controlled lighting, sounds, textures to touch, and scents—along with support from a therapist.
The results showed that combining the sensory room experience with therapist support worked better than either approach alone. Participants reported less pain (especially after several sessions), along with lower blood pressure, greater life satisfaction, and reduced anxiety.
The key insight from this study is that engaging multiple senses at once helps the brain process pain differently. This offers those of us with chronic pain a drug-free option that doesn't require special equipment beyond a therapeutic environment.
2. Visualization and Mindful Reprogramming
A 2021 study in the International Journal of Rheumatic Diseases tested a deceptively simple idea: what if you could retrain your brain to produce less pain?
Researchers worked with fibromyalgia patients over six weeks, teaching them to reconceptualize their pain as a modifiable brain output rather than fixed tissue damage, incorporating simple mental exercises to "quiet" overactive signals
The results were measurable: pain impact scores dropped significantly, fear of movement decreased, and patients could tolerate more pressure on tender points across their bodies. These improvements lasted at least three months. Patients reported their pain dropping by 20-30% on average, and many kept improving even after the study ended.
3. Brain Games Train Pain Away
A small 2025 pilot study in Frontiers in Pain Research took this a step further by adding real-time brain feedback. Participants wore portable EEG sensors at home and played simple "games" that involved inflating virtual balloons or completing puzzles that responded to their actual brainwave patterns. The goal was to increase calming alpha rhythms in the brain's sensory processing area, essentially learning to "dim" the pain signal at its source.
Over eight weeks (40 sessions), they practiced visualizing their neural activity settling down, and the technology confirmed when they succeeded. More than half experienced clinically meaningful relief—at least 30% pain reduction—with brain measurements supporting the changes with more calming alpha/theta waves and less agitated high-beta activity.
Why This Isn't Just "Positive Thinking"
This isn't about pretending pain doesn't exist or willing it away; it's about leveraging the brain's ability to rewire itself based on what you repeatedly practice.
The key to this biofeedback model is maintaining focus on targeted visualization during these mindfulness exercises, envisioning the pain centers in your brain and instructing them to reduce their pain output signalling.
Central to this approach is Moskowitz's MIRROR framework:
Motivation: Establishing a deep, personal "why" to fuel commitment, as pain rewiring demands overriding habitual neural firing patterns that have dominated for years.
Intention: Precise focus on specific brain regions (e.g., visualizing S1 pain maps shrinking), directing attention to induce targeted synaptic weakening.
Relentlessness: Persistent daily practice, often 1-2 hours, to outcompete pain signals; Moskowitz cured his own 13-year neck pain through visualization after conventional treatments failed.
Repetition: Frequent reinforcement strengthens new adaptive circuits, reversing overactive nerve signals and preventing rebound pain.
Observation: By calmly noticing how your pain changes, you can better monitor the progress of your neural recalibration without getting emotionally pulled in.
Reward: Celebrating incremental victories boosts dopamine and enhances prefrontal regulation of pain signals.
Anytime your brain is being stimulated with a pain signal, you need to counter-stimulate it, otherwise you give the neurons the opportunity to strengthen those pathways. These therapies compete with the same areas of the brain that have been recruited to pain processing, ultimately reducing the hypersensitivity.
Expert Perspectives on Chronic Pain
Chronic pain is not an immutable sentence but a challenge that can be systematically addressed. By understanding our brain's remarkable plasticity and implementing targeted, holistic strategies, remarkable transformations become possible. My personal journey intersects with a growing body of research highlighting the profound connection between our psychological state and the manifestation of physical pain.
Moskowitz is but one among a remarkable group of thought leaders who have pioneered groundbreaking approaches to alleviating human suffering. Pioneers like Dr. John Sarno, Dr. Howard Schubiner, and Dr. David Burns have consistently highlighted the profound connection between psychological states and physical pain.
Dr. David Burns, a Stanford psychiatrist, explores emotional healing in Feeling Good, while Dr. Fred Luskin's research on forgiveness at Stanford, detailed in Forgive for Good, offers transformative insights into emotional resilience. Dr. Steven Porges's Polyvagal Theory provides additional scientific validation, demonstrating how our nervous system's intricate mechanisms fundamentally influence physical and emotional well-being.
All these experts converge on a powerful central insight: healing emerges from our innate capacity to create internal safety and optimize our body's biochemical responses. By understanding and engaging with our body's natural healing capacities, we can unlock remarkable potential for transformation and health.
The Healing Potential: A Message of Hope
If you're interested, you can read a free excerpt of The Brain's Way of Healing by Norman Doidge here.
This chapter outlines Moskowitz's brain mapping protocol in greater detail and features a compelling case study demonstrating its effectiveness. Or, if you want to be inspired by incredible stories of healing using groundbreaking neurological principles, you can explore some of these other resources for deeper exploration of the topic:
The Way Out by Alan Gordon
Mind Over Back Pain by Dr. John Sarno
Unlearn Your Pain by Dr. Howard Schubiner
Back in Control by Dr. David Hanscomb
Your Journey to Pain Relief
My journey continues, marked not by complete elimination of pain, but by increasing moments of relief and a profound respect for the body's inherent healing capacities.
Healing requires both surrender and effort: accepting where you are while gently testing what's possible with adaptation and compassionate self-exploration. Our bodies possess extraordinary capabilities, and we need only learn to listen, understand, and gently guide them toward wellness.
Please note: Some of the links in this article are affiliate links. If you make a purchase through these links, we may earn a small commission at no additional cost to you. Your support helps Grassroots Vitality continue to provide valuable content. Thank you!
Bibliography
Burns, D. D. (1980). Feeling good: The new mood therapy. William Morrow.
Doidge, N. (2015). The brain's way of healing: Remarkable discoveries and recoveries from the frontiers of neuroplasticity. Viking. (Chapter 1 details Michael Moskowitz's approach to chronic pain through visualization and neuroplasticity.)
Gordon, A., & Ziv, A. (2021). The way out: A revolutionary, scientifically proven approach to healing chronic pain. Avery.
Hanscom, D. (2012). Back in control: A spine surgeon's roadmap out of chronic pain (2nd ed.). Vertus Press.
Khatib, S., Palgi, Y., Ashar, Y. K., Polyvyannaya, N., & Goldstein, P. (2025). The combined effect of multisensory stimulation and therapist support on physical and mental health of older adults living in nursing homes: Pilot randomized controlled trial. Journal of Medical Internet Research, 27, e55042. https://doi.org/10.2196/55042
Luskin, F. (2002). Forgive for good: A proven prescription for health and happiness. HarperOne.
Sarno, J. E. (1984). Mind over back pain: A radically new approach to the diagnosis and treatment of back pain. Berkley Books.
Sakel, M., Ozolins, C. A., Saunders, K., & Biswas, R. (2025). A home-based EEG neurofeedback treatment for chronic neuropathic pain—a pilot study. Frontiers in Pain Research, 6, Article 1479914. https://doi.org/10.3389/fpain.2025.1479914
Schubiner, H. (2022). Unlearn your pain (4th ed.). Mind Body Publishing.
Saracoglu, I., Leblebicier, M. A., Yaman, F., & Kavuncu, V. (2021). Pain neuroscience education combined with usual treatment for fibromyalgia syndrome: A randomized controlled trial. International Journal of Rheumatic Diseases, 24(11), 1409–1418.